Mental Disabilities

Duloxetine Systemic (Cymbalta):
Warning:
Oral route (Capsule, Delayed Release)
Antidepressants increased the risk of suicidal thinking and behavior in children, adolescents, and young adults in short-term studies.These studies did not show an increase in the risk of suicidal thoughts and behavior with antidepressant use in patients over age 24; there was a reduction in risk with antidepressant use in patients aged 65 or older.Closely monitor all antidepressant-treated patients for clinical worsening, and for emergence of suicidal thoughts and behaviors. Advise families and caregivers of the need for close observation and communication with the prescriber.
Side effects:
Asthenia
Constipation
Diarrhoea
Dizziness
Drowsiness
Fatigue
Hypersomnia
Insomnia
Nausea
Sedated state
Headache
Xerostomia
Other side effects include:
Agitation
Erectile dysfunction
Nervousness
Psychomotor agitation
Tension
Vomiting
Abdominal pain
Anorexia
Decreased appetite
Decreased libido
Hyperhidrosis
Loss of libido
Restlessness
Side effects requiring immediate medical attention:
Area rash
Blindness
Blistering, peeling, or loosening of the skin
Blurred vision
Change in consciousness
Chest tightness
Chills
Clay-colored stools
Cold sweats
Confusion
Dark urine
Decreased urine output
Difficulty with swallowing
Dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
Eye pain
Fainting
Fast or irregular heartbeat
General tiredness or weakness
Hives or welts, itching, or skin rash
Increased thirst
Joint or muscle pain
Large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
Light-colored stools
Loss of consciousness
Red skin lesions, often with a purple centre
Seizures
Sores, ulcers, or white spots in the mouth or on the lips
Stomach pain
Tearing
Unpleasant breath odour
Upper right stomach pain
Vomiting of blood
Yellow eyes and skin
Wellbutrin XL (Bupropion Systemic):
Warning:
Oral route (Tablet, Extended Release)
Suicidality and Antidepressant Drugs
Antidepressants increased the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short-term trials. These trials did not show an increase in the risk of suicidal thoughts and behavior with antidepressant use in subjects aged 65 and older.In patients of all ages who are started on antidepressant therapy, monitor closely for worsening, and for emergence of suicidal thoughts and behaviors. Advise families and caregivers of the need for close observation and communication with the prescriber.
Oral route (Tablet; Tablet, Extended Release)
Suicidality and Antidepressant Drugs
Although Zyban® is not indicated for treatment of depression, it contains the same active ingredient as the antidepressant medications Wellbutrin®, Wellbutrin® SR, and Wellbutrin XL®. Antidepressants increased the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short-term trials. These trials did not show an increase in the risk of suicidal thoughts and behavior with antidepressant use in subjects over age 24; there was a reduction in risk with antidepressant use in subjects aged 65 and older. In patients of all ages who are started on antidepressant therapy, monitor closely for worsening, and for emergence of suicidal thoughts and behaviors. Advise families and caregivers of the need for close observation and communication with the prescriber BuPROPion hydrochloride extended-release tablet is not approved for use in paediatric patients.
Side Effects:
Constipation
Decrease in appetite
Dizziness
Increased sweating
Stomach pain
Trembling
Unusual weight loss
Other side effects include:
Blurred vision
Change in sense of taste
Drowsiness
Frequent need to urinate
Sore throat
Unusual feeling of well-being
Side effects requiring immediate medical attention:
Anxiety
Dry mouth
Hyperventilation
Irregular heartbeats
Irritability
Restlessness
Shaking
Trouble sleeping
Buzzing or ringing in the ears
Headache (severe)
Skin rash, hives, or itching
Confusion
Fainting
False beliefs that cannot be changed by facts
Having extreme distrust of people
Seeing, hearing, or feeling things that are not there
Seizures
Trouble concentrating
Sertraline Systemic (Zoloft):
Warning:
Oral route (Solution; Tablet)
Antidepressants increased the risk of suicidal thoughts and behavior in pediatric and young adult patients in short-term studies. Closely monitor all antidepressant-treated patients for clinical worsening, and for emergence of suicidal thoughts and behaviors
Side Effects:
Acid or sour stomach
Belching
Decreased appetite or weight loss
Diarrhoea or loose stools
Heartburn
Sleepiness or unusual drowsiness
Stomach cramps, gas, or pain
Trouble sleeping
Other side effects include:
Agitation, anxiety, or nervousness
Bladder pain
burning, crawling, itching, numbness, prickling, "pins and needles", or tingling feelings
Changes in vision
Cloudy urine
Constipation
Difficult, burning, or painful urination
Flushing or redness of the skin, with feeling of warmth or heat
Frequent urge to urinate
Increased appetite
Pain or tenderness around the eyes and cheekbones
Stuffy or runny nose
Side effects requiring immediate medical attention:
Decreased interest in sexual intercourse
Failure to discharge semen (in men)
Inability to have or keep an erection
Loss in sexual ability, desire, drive, or performance
Aggressive reaction
Breast tenderness or enlargement
Confusion
Convulsions
Diarrhoea
Drowsiness
Dryness of the mouth
Fast talking and excited feelings or actions that are out of control
Fever
Inability to sit still
Increase in body movements
Increased sweating
Increased thirst
Lack of energy
Loss of bladder control
Mood or behaviour changes
Muscle spasm or jerking of all extremities
Nosebleeds
Overactive reflexes
Racing heartbeat
Red or purple spots on the skin
Restlessness
Shivering
Skin rash, hives, or itching
Sudden loss of consciousness
Unusual or sudden body or facial movements or postures
Unusual secretion of milk (in females)
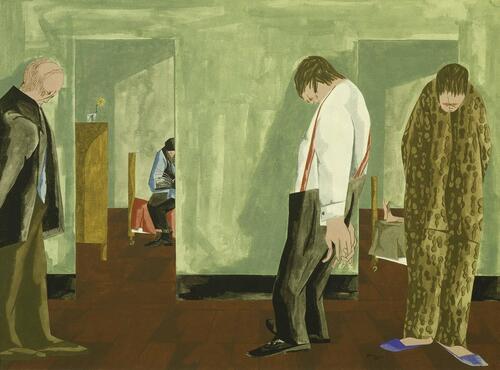
Jacob Lawrence:
Jacob Lawrence was a prominent African American artist and his work typically reflects his immersion in the Harlem Renaissance. His pieces struggle and show triumph. However, the images painted during his time in inpatient treatment are different. They show only struggle. Or perhaps, not even struggle, but rather humans succumbing to agony and defeat.
The garish colors of his fellow patients aren't entirely featureless; unlike most of his subjects, their features suggest that these are white people. In fact, Lawrence was struggling with some important questions about race when he fell into the depression that caused him to check himself into a Queens psychiatric hospital. He was accepted as a black artist in a white world, but he questioned why that he was. Why had others not been accepted? Where were his black peers? He felt isolated, alone, and confused. Nine months later, when he was released, his Hospital series garnered a lot of attention. A mostly white art world said it was his best work. Ebony magazine questioned whether this was subtle racism; did they critics like the work better because it reflected white reality, even if it was the reality of people in a mental hospital?
Regardless, the hospital stay helped Lawrence. He said that getting guidance to better understand his own personality and nature was one of the deepest experiences of his life. Plus he gave a shout out to his wife (painter Gwendolyn Knight) for her unwavering support during his stay.
With depression, people might experience a single depressive period, or they might suffer from chronic relapse. In Lawrence’s case, he spent nine months in inpatient treatment, after which he thrived.
Henri de Toulouse-Lautrec:
Woman Pulling Up Her Stocking at the Toulouse-Lautrec Museum
Perhaps one of the reasons that Toulouse-Lautrec painted depression in Jane’s face was because it was something he recognized from his own experience. In fact, Jane wasn’t the only one that he portrayed this way. An examination of his 700+ paintings and 5,000 drawings reveals that, as Michael Kimmelman put it in a 1992 New York Times article, “over and over again, Lautrec turned out images of alienation, joylessness, and ennui.”
Tracey Emin “My Bed” 1998:
Elise J. M. Pacquette:
Protecting the Heart 1993
Pacquette's art acts as a window into the lived experience of a mental health condition. This lends it the ability to engender empathy from those without similar experiences, solace for those who do and – as with many of the artworks discussed above – a surprising and poignant note of hope.
William Doan, video animation:
Alex Billington, video animation:
https://www.firstshowing.net/2020/watch-powerful-how-to-float-short-film-about-anxiety-depression/
Recreation ''the sauna'' (2021):

fluoxetine systemic (Prozac):
Warning
Oral route (Capsule; Capsule, Delayed Release)
Antidepressants can increase the risk of suicidal thinking and behavior in children, adolescents, and young adults with major depressive disorder. Closely monitor patients of all ages for clinical worsening and emergence of suicidal thoughts and behaviors. When using fluoxetine hydrochloride and olanzapine in combination, also refer to the Boxed Warning section of the package insert for fluoxetine hydrochloride/olanzapine.
Oral route (Solution)
Antidepressants can increase the risk of suicidal thinking and behavior in children, adolescents, and young adults with major depressive disorder (MDD). Closely monitor patients of all ages for clinical worsening and emergence of suicidal thoughts and behaviors. Fluoxetine oral solution is approved for use in pediatric patients with MDD and obsessive compulsive disorder.
Oral route (Tablet)
Antidepressants can increase the risk of suicidal thinking and behavior in children, adolescents, and young adults with major depressive disorder. Closely monitor patients of all ages for clinical worsening and emergence of suicidal thoughts and behaviors. Fluoxetine hydrochloride oral tablets are not approved for use in pediatric patients.
Side effects:
Decreased appetite
Abnormal dreams
breast enlargement or pain
change in sense of taste
changes in vision
feeling of warmth or heat
flushing or redness of the skin, especially on face and neck
frequent urination
hair loss
increased appetite
increased sensitivity of the skin to sunlight
menstrual pain
stomach cramps, gas, or pain
unusual secretion of milk, in females
weight loss
yawning
Other side effects:
Cracks in the skin
loss of heat from the body
painful or prolonged erections of the penis
scaly skin
swelling of the breasts or breast soreness in both females and males
unusual milk production
Side effects requiring immediate medical attention:
Hives, itching, skin rash
inability to sit still
restlessness
Chills or fever
joint or muscle pain
Anxiety
cold sweats
confusion
cool pale skin
diarrhea
difficulty with concentration
drowsiness
dryness of the mouth
excessive hunger
fast or irregular heartbeat
headache
increased sweating
increased thirst
lack of energy
mood or behavior changes
overactive reflexes
purple or red spots on the skin
racing heartbeat
seizures
shakiness or unsteady walk
shivering or shaking
talking, feeling, and acting with excitement and activity you cannot control
trouble with breathing
unusual or incomplete body or facial movements
unusual tiredness or weakness
Venlafaxine Systemic (Effexor XR):
Warning
Oral route (Capsule, Extended Release)
Antidepressants increased the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short-term studies. These studies did not show an increase in the risk of suicidal thoughts and behavior with antidepressant use in patients older than 24 years; there was a reduction in risk with antidepressant use in patients aged 65 or older. In patients of all ages who are started on antidepressant therapy monitor closely for clinical worsening and emergence of suicidal thoughts and behaviors. Venlafaxine is not approved for use in pediatric patients.
Oral route (Tablet; Tablet, Extended Release)
Antidepressants increased the risk of suicidal thinking and behavior in children, adolescents, and young adults in short-term studies with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults older than 24 years, and there was a reduction in risk with antidepressants compared with placebo in adults aged 65 or older. This risk must be balanced with the clinical need. Monitor patients closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. Not approved for use in pediatric patients
Side Effects:
Abnormal dreams
chills
constipation
decrease in sexual desire or ability
diarrhea
dry mouth
heartburn
increased sweating
loss of appetite
nausea
stomach pain or gas
stuffy or runny nose
tingling, burning, or prickly sensations
trouble sleeping
vomiting
weight loss
Other Side Effects:
Change in taste
muscle tension
yawning
Side effects requiring immediate medical attention:
Change or problem with discharge of semen
decreased interest in sexual intercourse
inability to have or keep an erection
lack or loss of strength
loss in sexual ability, desire, drive, or performance
severe headache
sweating
Blurred vision
chest pain
delayed or inability to have an orgasm
fast or irregular heartbeat
mood or mental changes
ringing or buzzing in the ears
suicidal thoughts
Actions that are out of control
high fever
irritability
itching or skin rash
lightheadedness or fainting, especially when getting up suddenly from a sitting or lying position
menstrual changes
nervousness
problems with urinating or holding urine
seizures
severe muscle stiffness
talking, feeling, and acting with excitement that you cannot control
trouble breathing
unusually pale skin
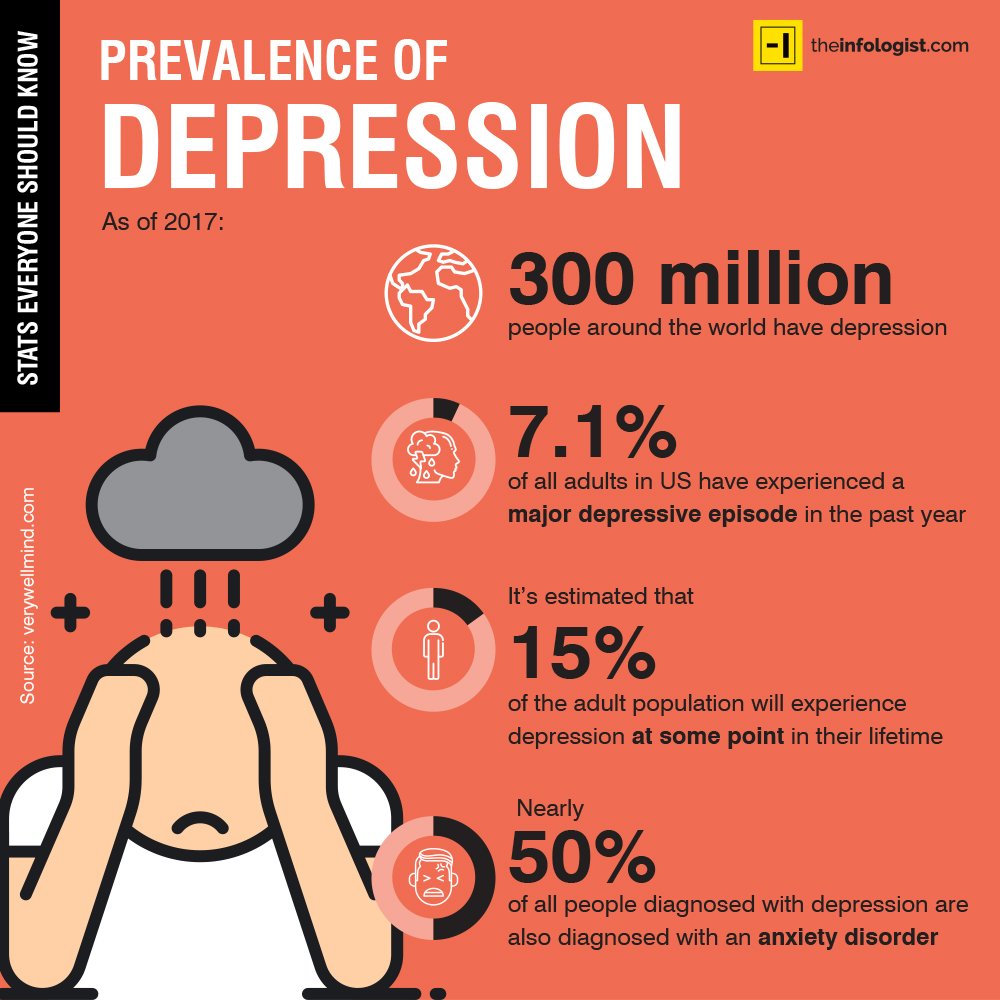
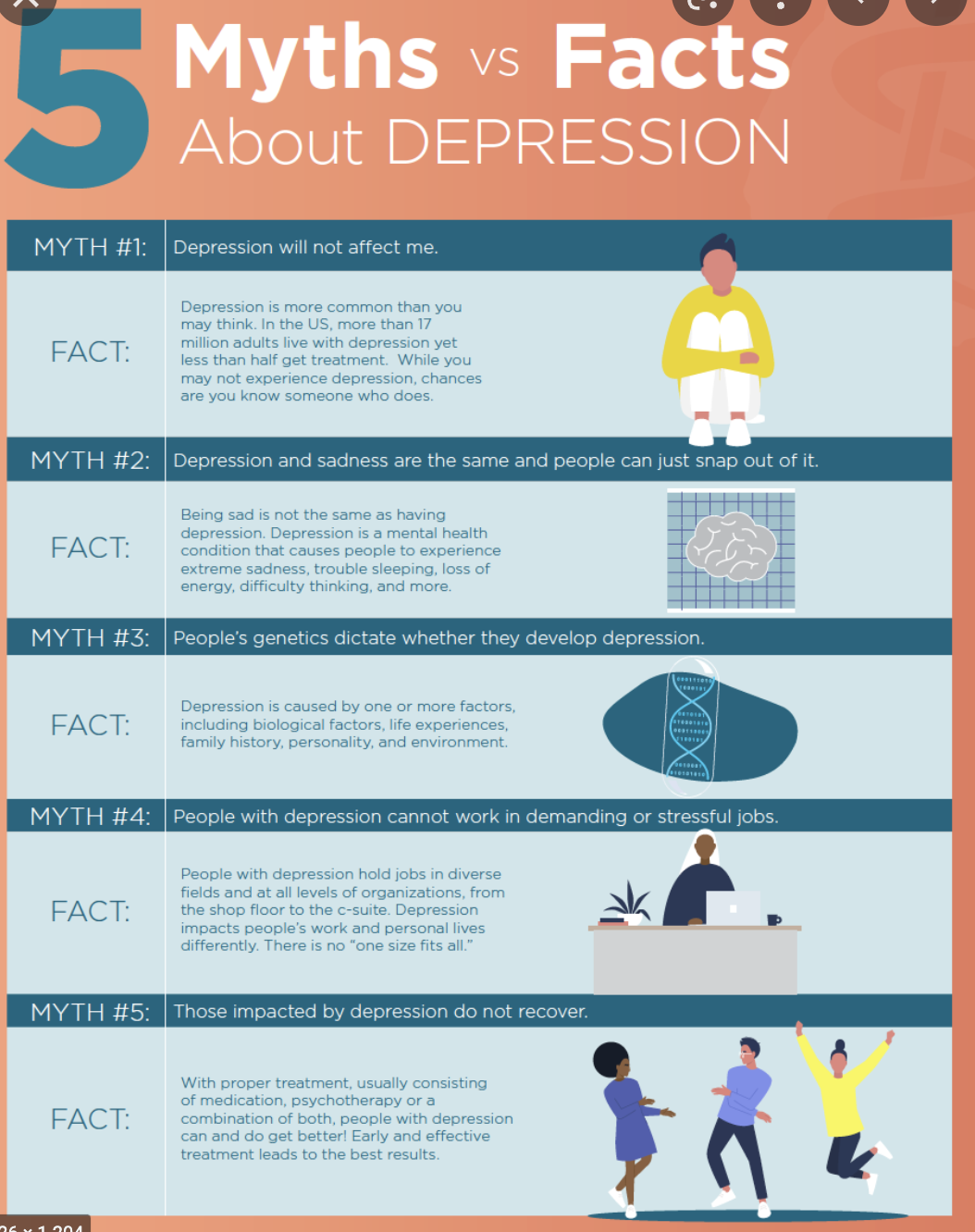
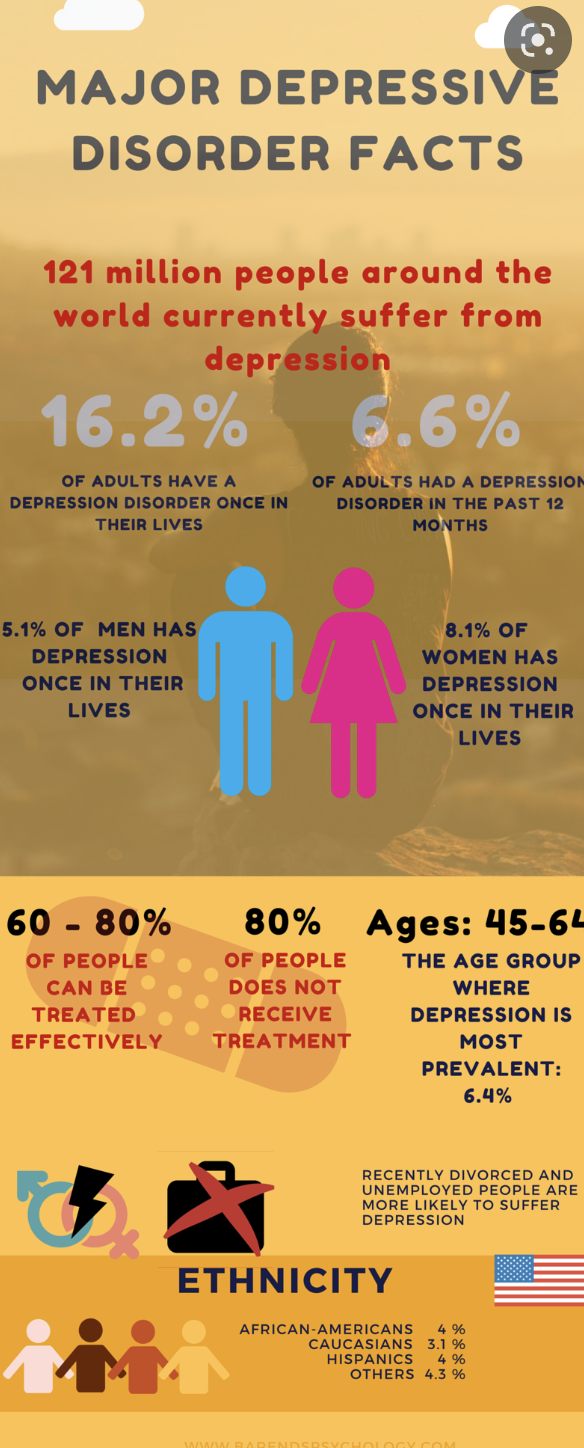
WHAT IS DEPRESSION AND FACTS ABOUT IT
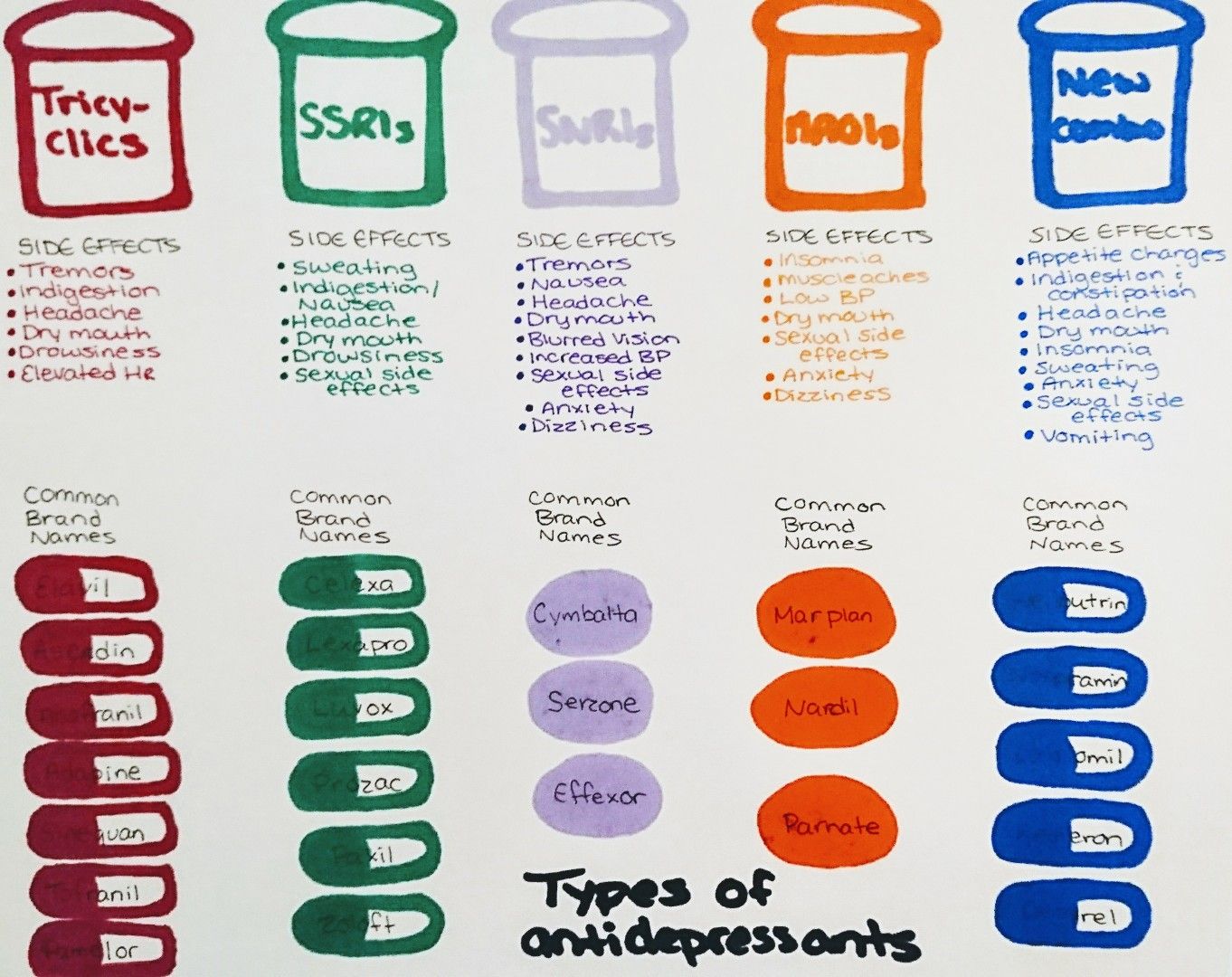
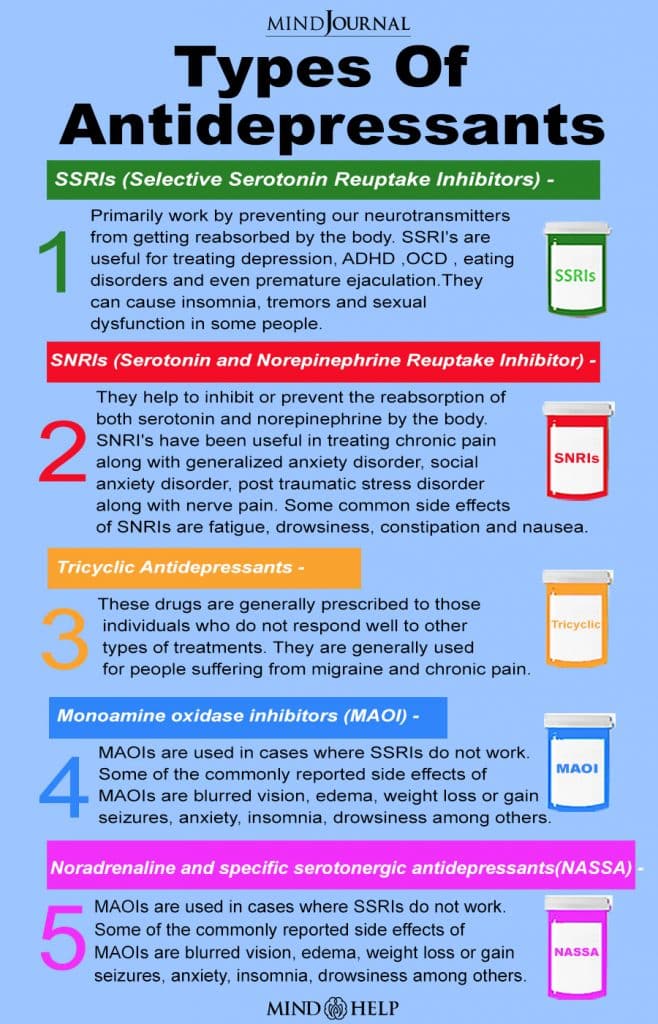
WHAT ARE ANTIDEPRESSANTS AND THEIR TYPES
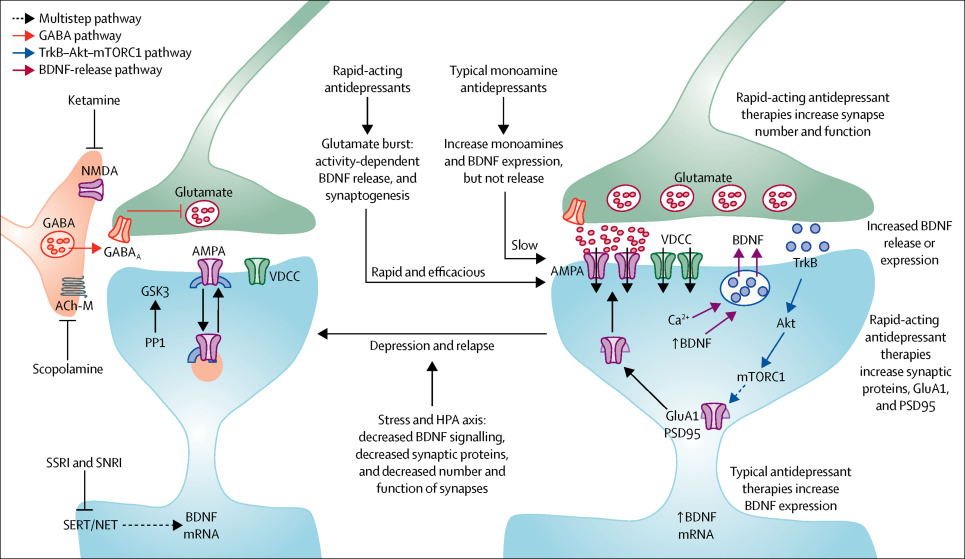
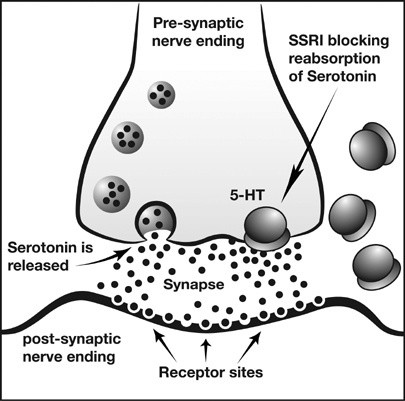
HOW DO ANTIDEPRESSANTS WORK?
WHAT DID ARTISTS DO ABOUT THIS TOPIC
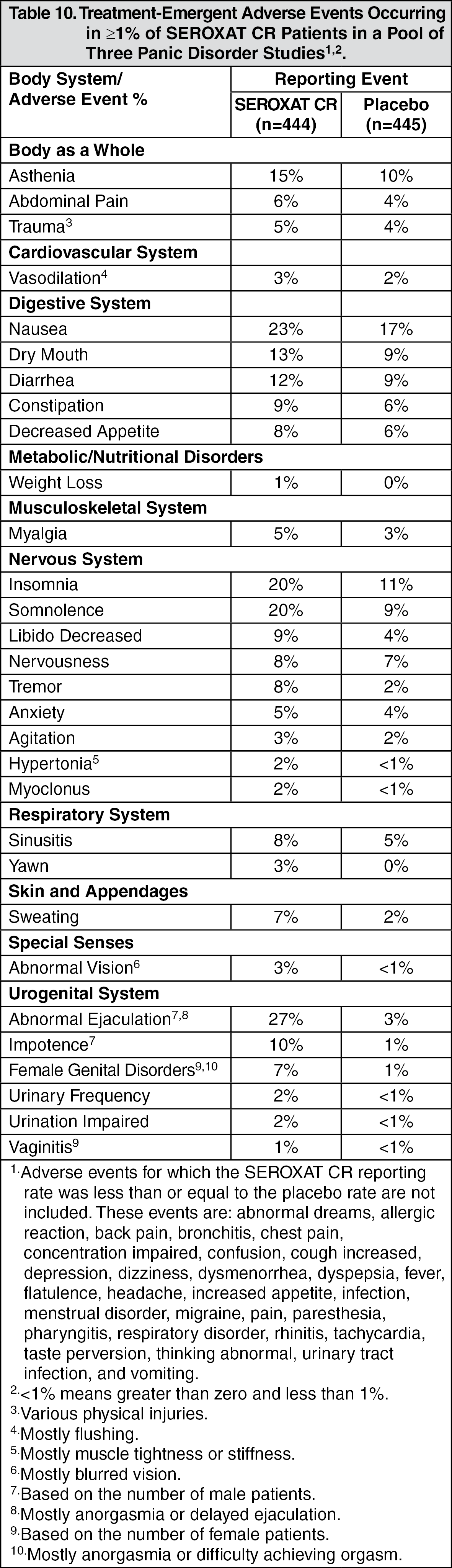
SIDE EFFECTS OF THE POPULAR MEDICATION
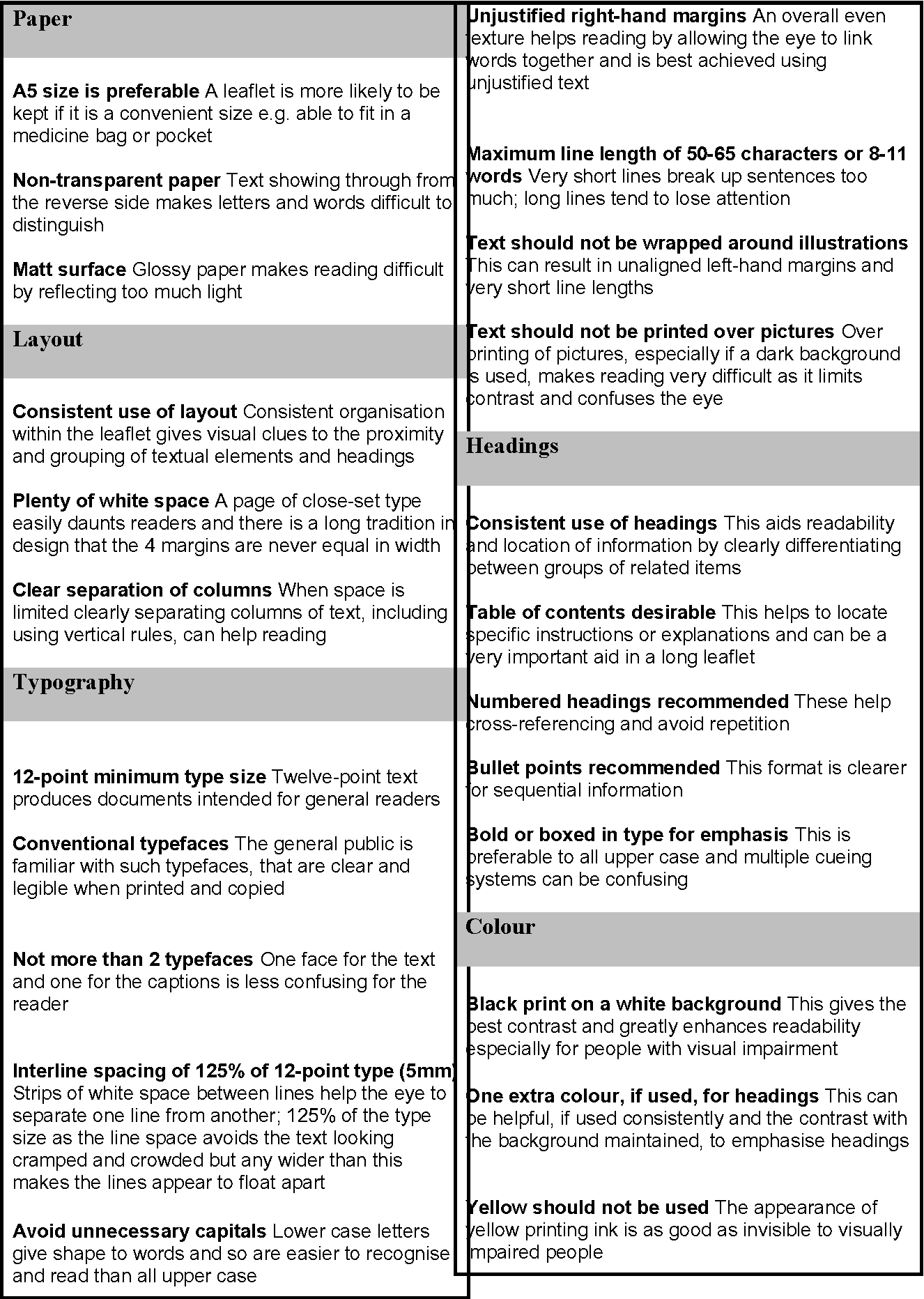
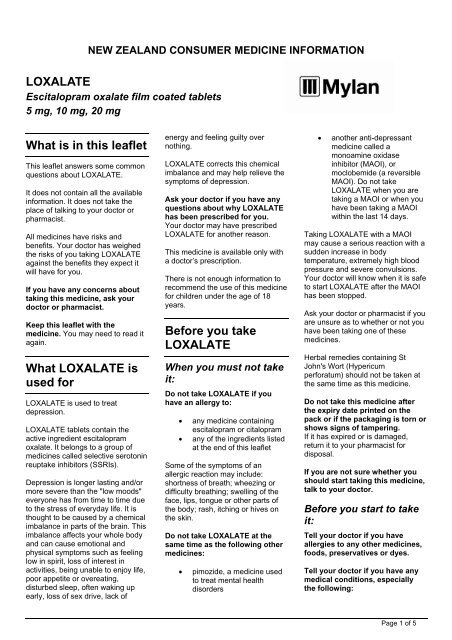
patient information leaflet examples (for the presentation)
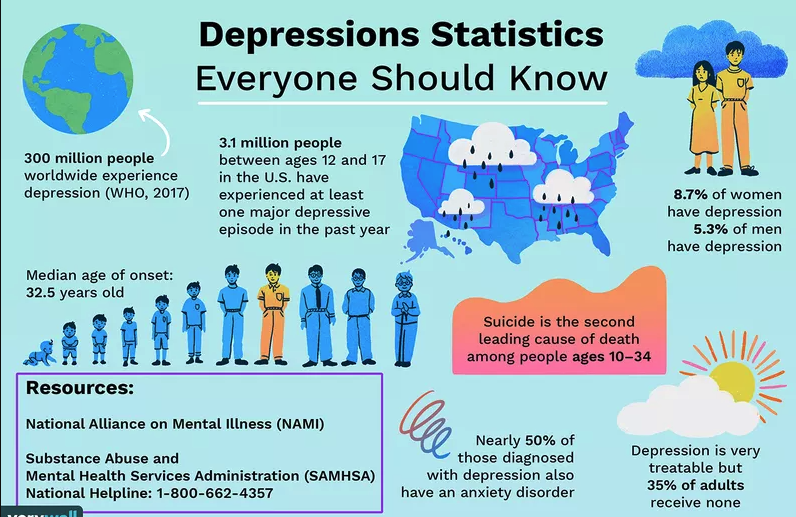
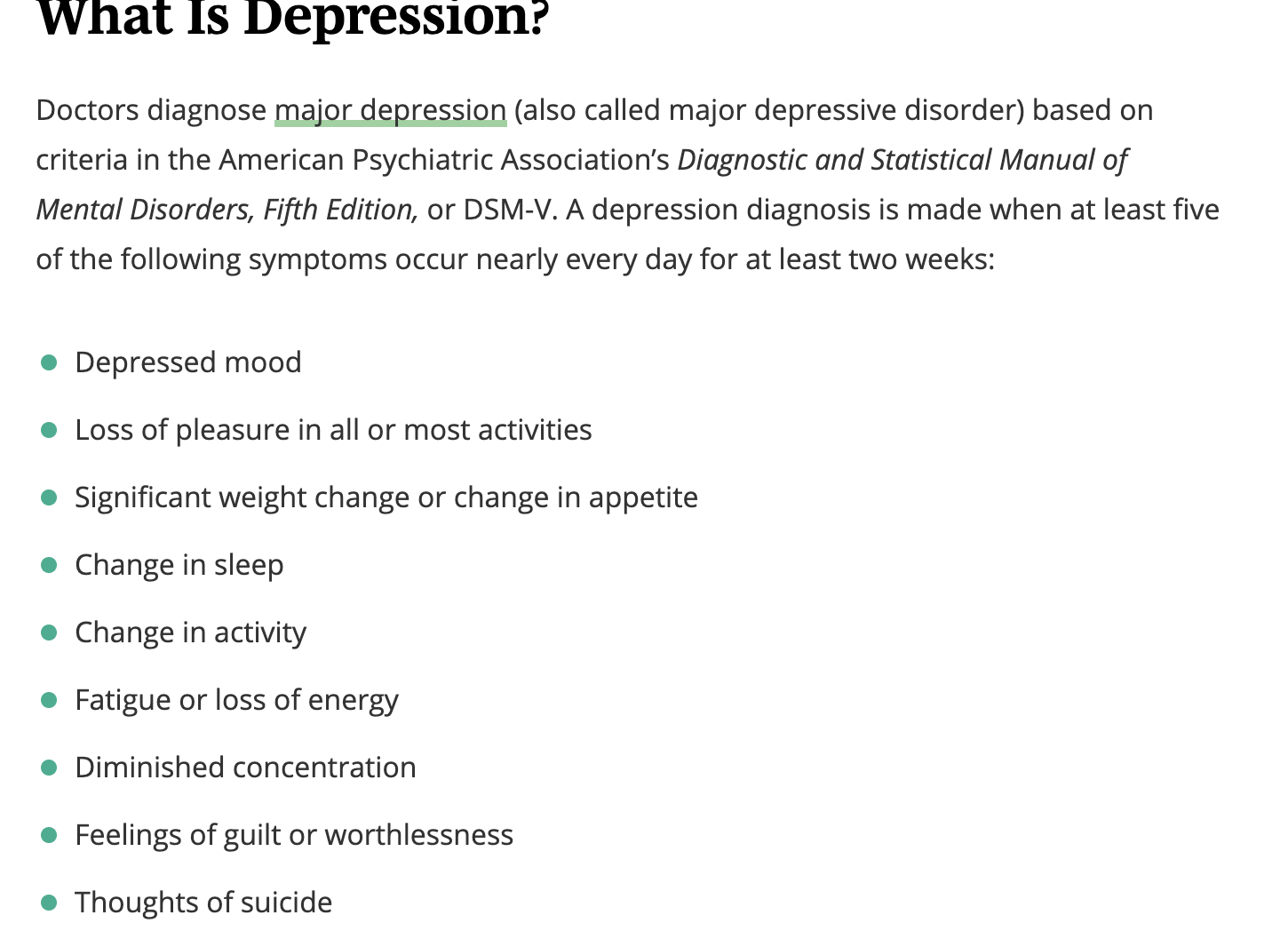
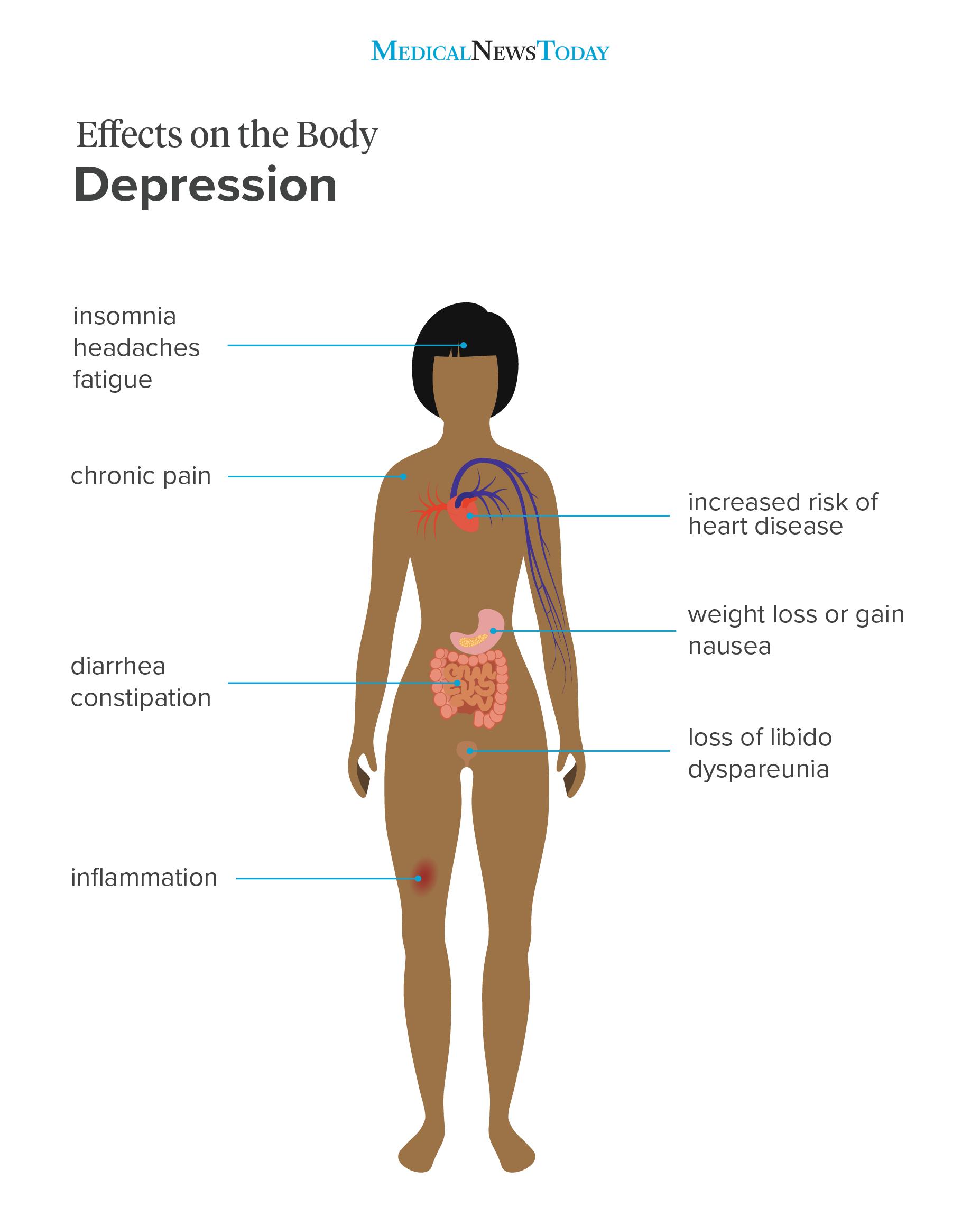
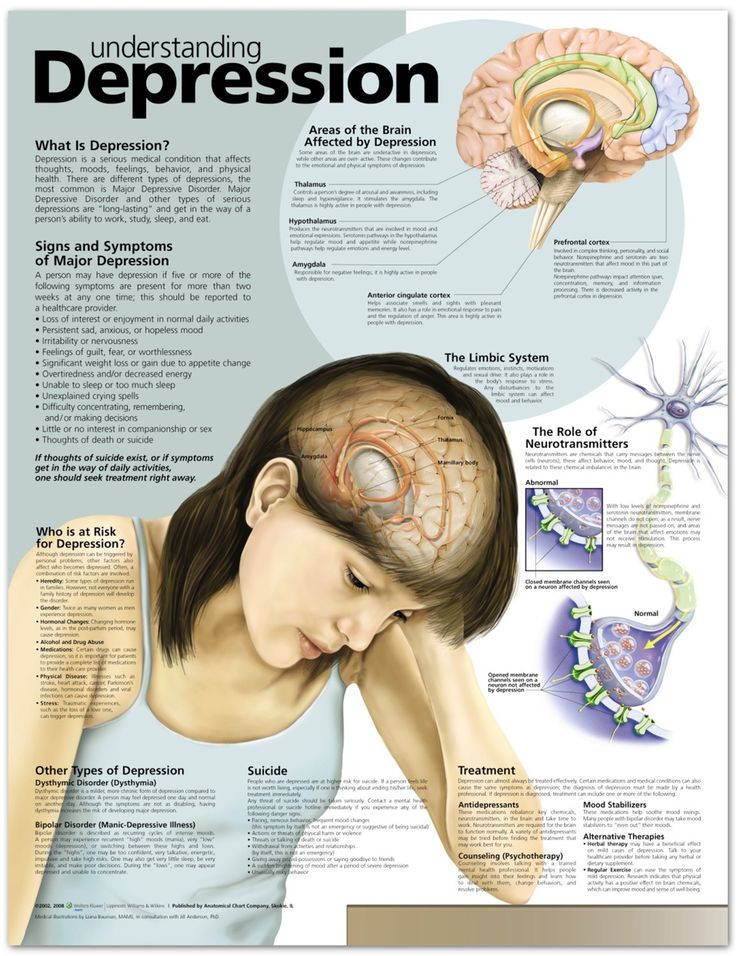
Depression (major depressive disorder) is a common and serious medical illness that negatively affects how you feel, the way you think and how you act. Fortunately, it is also treatable. Depression causes feelings of sadness and/or a loss of interest in activities you once enjoyed. It can lead to a variety of emotional and physical problems and can decrease your ability to function at work and at home.
Depression symptoms can vary from mild to severe and can include:
Feeling sad or having a depressed mood
Loss of interest or pleasure in activities once enjoyed
Changes in appetite — weight loss or gain unrelated to dieting
Trouble sleeping or sleeping too much
Loss of energy or increased fatigue
Increase in purposeless physical activity (e.g., inability to sit still, pacing, handwringing) or slowed movements or speech (these actions must be severe enough to be observable by others)
Feeling worthless or guilty
Difficulty thinking, concentrating or making decisions
Thoughts of death or suicide
Symptoms must last at least two weeks and must represent a change in your previous level of functioning for a diagnosis of depression.
Also, medical conditions (e.g., thyroid problems, a brain tumor or vitamin deficiency) can mimic symptoms of depression so it is important to rule out general medical causes.
Depression affects an estimated one in 15 adults (6.7%) in any given year. And one in six people (16.6%) will experience depression at some time in their life. Depression can occur at any time, but on average, first appears during the late teens to mid-20s. Women are more likely than men to experience depression. Some studies show that one-third of women will experience a major depressive episode in their lifetime. There is a high degree of heritability (approximately 40%) when first-degree relatives (parents/children/siblings) have depression.
https://psychiatry.org/patients-families/depression/what-is-depression
If you’re being treated for depression, taking an antidepressant may be part of your treatment plan. Antidepressants work by balancing chemicals in your brain called neurotransmitters that affect mood and emotions. These depression medicines can help improve your mood, help you sleep better, and increase your appetite and concentration.
https://www.webmd.com/depression/features/antidepres
sant-effects#:~:text=Antidep
ressants%20wor
k%20by%20b
alancing%20chemicals,increase%20
your%20appetite%20and%20concentration.
If you've read up on antidepressants -- in newspapers and magazines, or on the Web -- you might see depression explained simply as a "chemical imbalance" or a "serotonin deficiency." Unfortunately, it's not that simple. We really don't know what causes depression or how it affects the brain. We don't exactly know how antidepressants improve the symptoms.
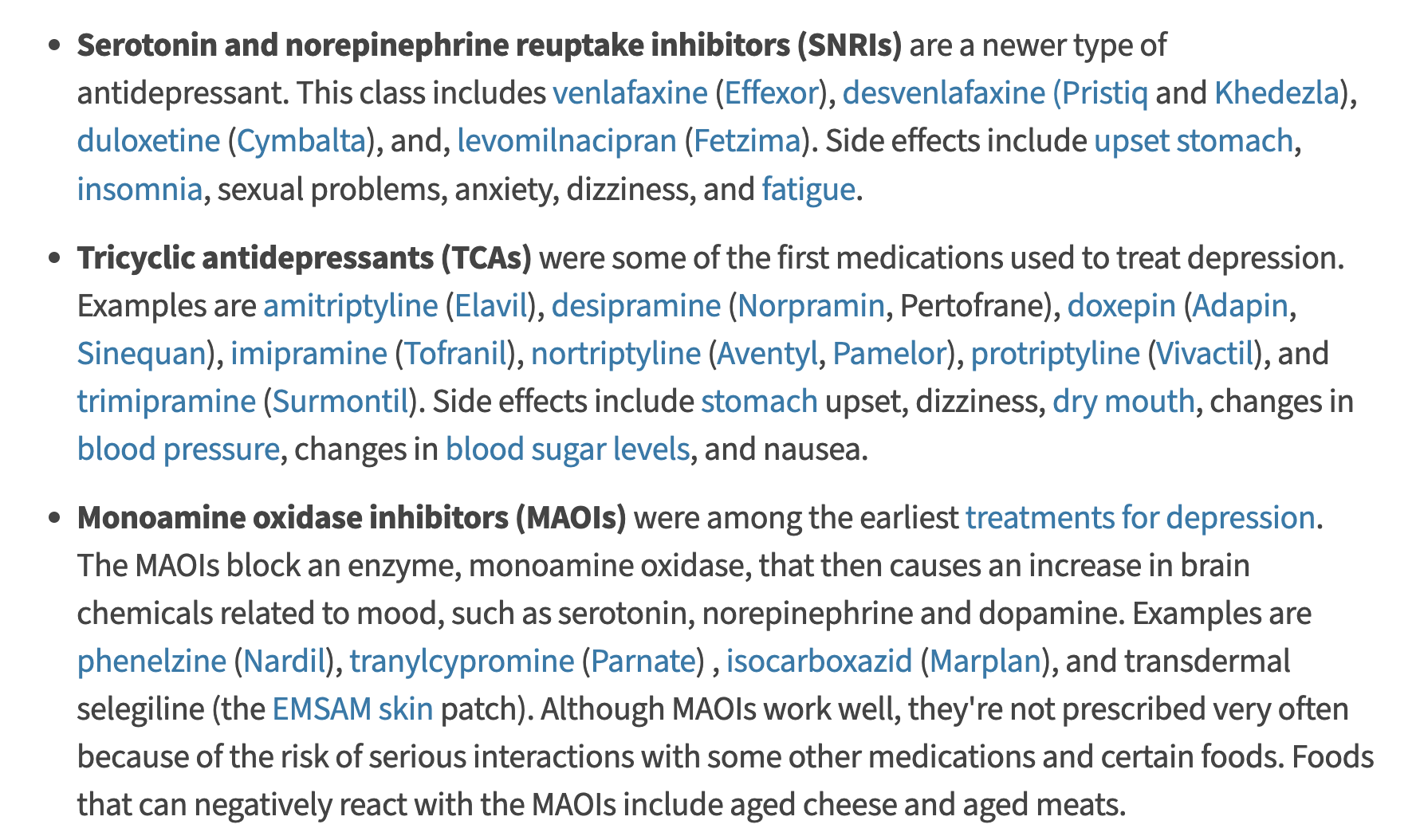
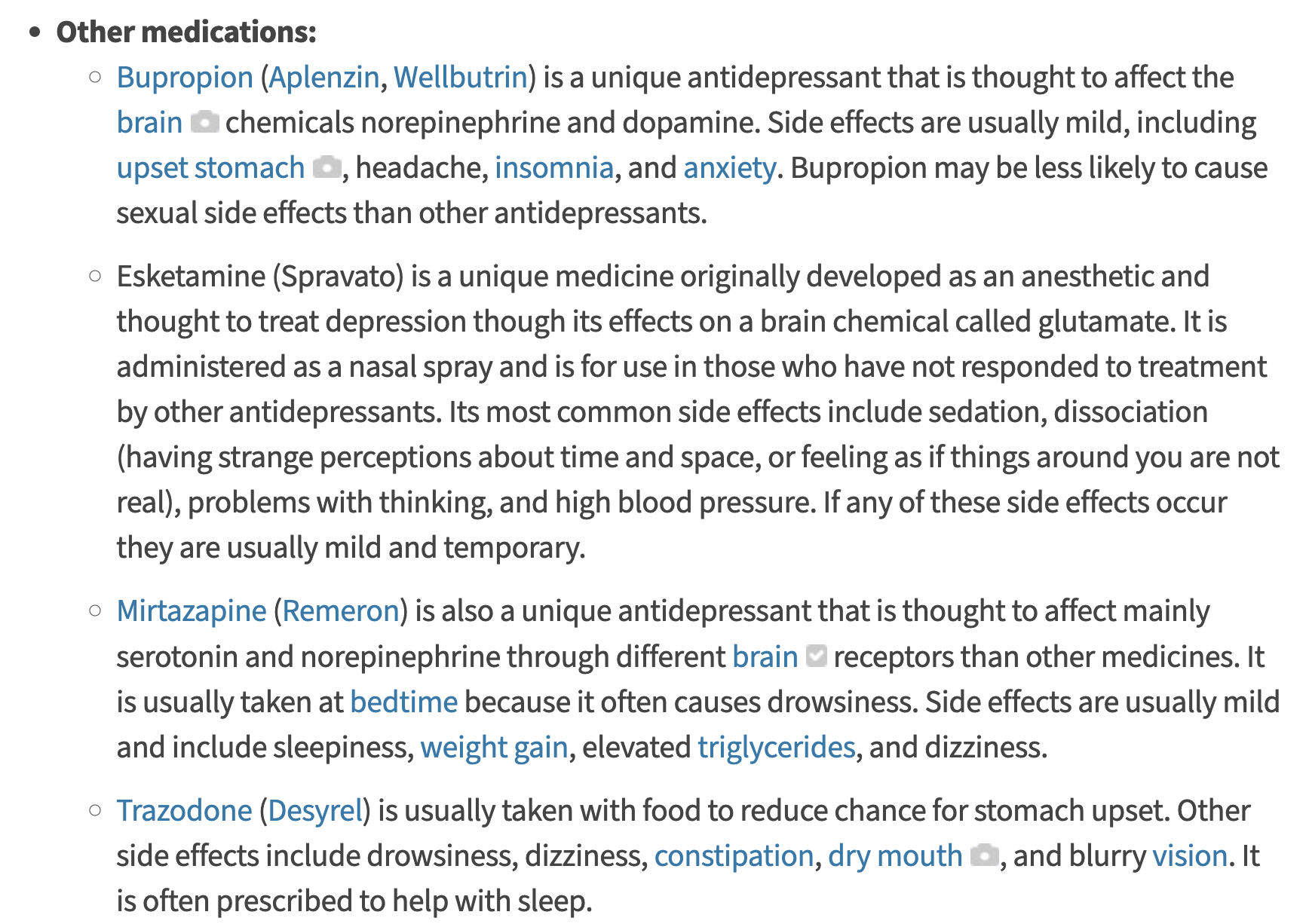
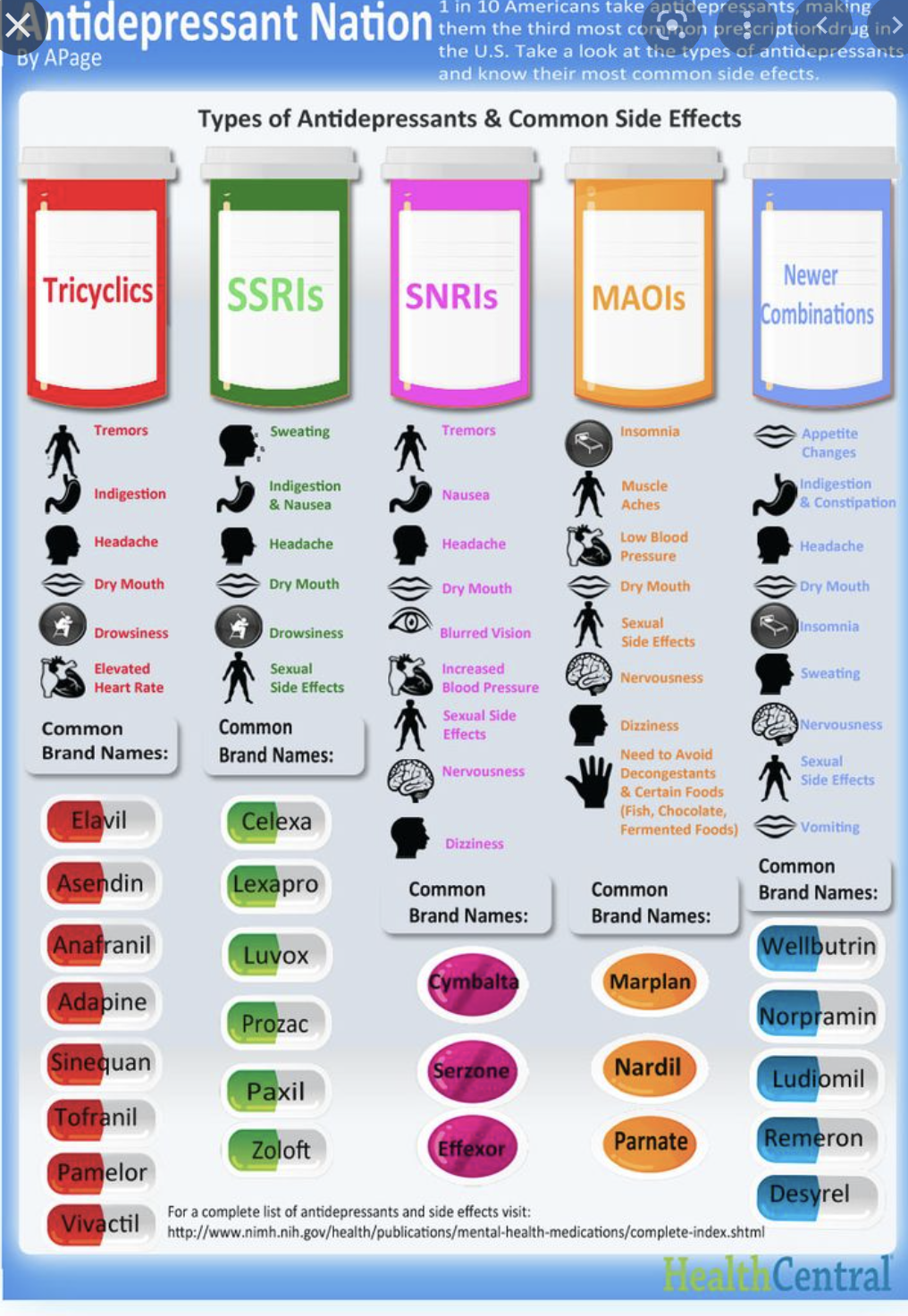
That said, many researchers believe that the benefits of antidepressants stem from how they affect certain brain circuits and the chemicals (called neurotransmitters) that pass along signals from one nerve cell to another in the brain. These chemicals include serotonin, dopamine, and norepinephrine. In various ways, different antidepressants seem to affect how these neurotransmitters behave. Here's a rundown of the main types of antidepressants.
https://www.webmd.com/depression/how-different-antidepressants-work
What are antidepressants?
Antidepressants are psychiatric drugs which are licensed to treat depression. Some are also licensed to treat other conditions, such as:
anxiety disorders
phobias
bulimia (an eating disorder)
some physical conditions, including managing long-term pain.
Who can prescribe antidepressants?
The healthcare professionals who can prescribe you antidepressants include:
your doctor (GP)
a psychiatrist
a specialist nurse prescriber
a specialist pharmacist.
https://www.mind.org.uk/information-support/drugs-and-treatments/antidepressants/about-antidepressants/
Antidepressants work by boosting the activity of particular brain chemicals, or making the activity last longer. This includes noradrenaline and serotonin, which are thought to be involved in regulating your mood.
https://www.mind.org.uk/information-support/drugs-and-treatments/antidepressants/about-antidepressants/
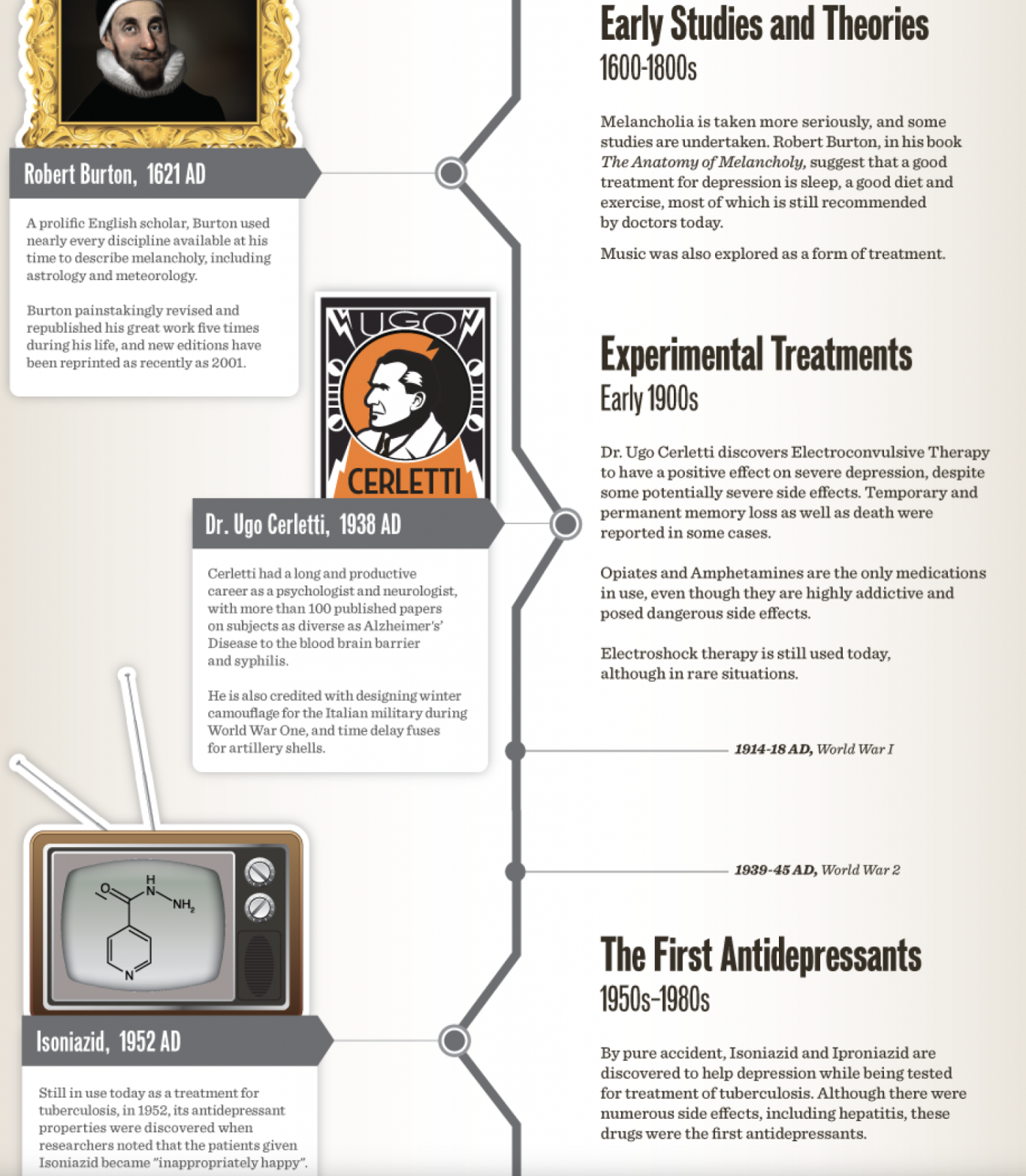
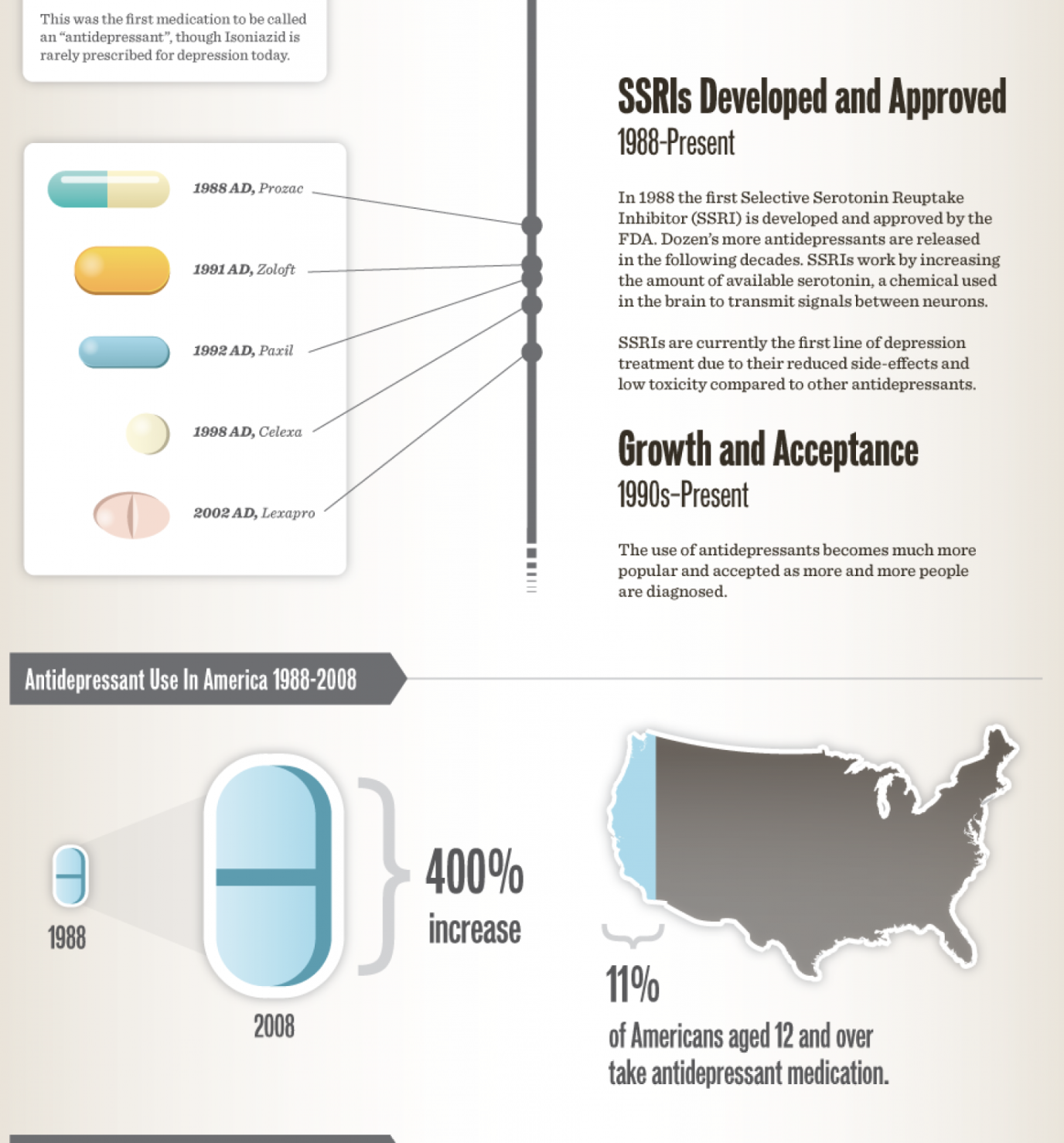
HISTORY OF ANTIDEPRESSANTS
https://www.greenbrooktms.com/blog/the-history-of-antidepressants#:~:text=The%20history%20of%20antidepressants%20began,dramatic%20change%
20in%20well%2Dbeing.
In the early 1970s, evidence for the role of serotonin in depression was gathering just as concerns were growing about the side effects of MAO inhibitors and tricyclic antidepressants.
Scientists thus turned their attention to SSRIs , or selective serotonin reuptake inhibitors. These drugs enhanced serotonin activity and seemed to carry fewer side effects than other antidepressants. A famous development in the history of antidepressants, fluoxetine was approved by the FDA in 1987 and reached the market the following year as Prozac ® . A year later, almost 2.5 million prescriptions had been dispensed. Other SSRIs since released include paroxetine, sertraline, citalopram, escitalopram, and fluvoxamine.
In the 1980s and 1990s, new antidepressants that targeted the monoamine neurotransmitter system emerged, including bupropion (a dopamine-norepinephrine reuptake inhibitor) and venlafaxine (a serotonin-norepinephrine reuptake inhibitor).
Despite these advances, any history of depression treatment must admit to several drawbacks related to these medications. All antidepressants can carry side effects, including nausea, dizziness, insomnia, and sexual dysfunction. They usually take several weeks to take effect. Up to a third of people with depression don't respond to these drugs . These shortcomings meant a new era of depression treatment was needed.
The clinical introduction of the first two specifically antidepressant drugs took place during the 1950s: iproniazid, a monoamine-oxidase inhibitor that had been used in the treatment of tuberculosis, and imipramine, the first drug in the tricyclic antidepressant family. Both antidepressant drugs made two fundamental contributions to the development of psychiatry: one of a social-health nature, consisting in an authentic change in the psychiatric care of depressive patients; and the other of a purely pharmacological nature, since these agents have constituted an indispensable research tool for neurobiology and psychopharmacology, permitting, among other things, the postulation of the first aetiopathogenic hypotheses of depressive disorders. The clinical introduction of fluoxetine, a selective serotonin reuptake inhibitor, in the late 1980s, once again revolutionized therapy for depression, opening the way for new families of antidepressants. All of these antidepressants, like the rest of those currently available for clinical practice, except agomelatine, share the same action mechanism, which involves the modulation of monoaminergic neurotransmission at a synaptic level. However, the future of antidepressant therapy could be directed to the search of extraneuronal non-aminergic mechanisms or mechanisms that modulate the intraneuronal biochemical pathways.
https://link.springer.com/chapter/10.1007/978-81-322-2803-5_26
Until the 1950s, opioids and amphetamines were the common drugs used as antidepressants. Due to their addictive nature, scientists and doctors ceased their use after two specifically antidepressant drugs were discovered accidentally: iproniazid and imipramine. (Lopez-Munoz and Alamo, 2009)
In 1951, scientist Hoffman-LaRoche developed iproniazid. This drug was originally meant to be used as an anti-tuberculosis drug however it was tested to give no results in treating tuberculosis. Further research found that it was useful in other applications, such as a psychic energizer (in the words of Nathan S.Kline). At first, the side effects such as feelings of euphoria, pain relief and increased mental alertness, were not considered therapeutic as they seemed to not have consistency in results. However, a trial carried out in 1958 by Loomer, Saunders, and Kline found a significant improvement in the treatment of depressive states. (FELDSTEIN, HOAGLAND and FREEMAN, 1959) In the 1960s however, the drug was retracted as lethal liver injury was found as a side effect.
https://imperialbiosciencereview.com/2020/10/30/the-history-of-antidepressants-discovery-and-development/
Also in the 1950s the first tricyclic antidepressants were discovered. These agents, so called because they are composed chemically of three carbon rings, inhibit the active reuptake, to varying degrees, of norepinephrine, serotonin, and dopamine in the brain. The tricyclics include imipramine, amitriptyline, desipramine, nortriptyline, and a number of other compounds. These drugs relieve symptoms in a high proportion (more than 70 percent) of depressed patients. As with the MAOIs, the antidepressant action of tricyclic drugs may not become apparent until two to four weeks after treatment begins.
SSRIs were introduced in the 1980s, and shortly thereafter they became some of the most commonly used antidepressants, primarily because they have fewer side effects than tricyclics or MAOIs. SSRIs include fluoxetine (Prozac), paroxetine (Paxil), and sertraline (Zoloft). SSRIs are also used in the treatment of anxiety, eating disorders, panic disorder, obsessive-compulsive disorder, and borderline personality disorder.
https://www.britannica.com/science/antidepressant
Scientists thus turned their attention to SSRIs , or selective serotonin reuptake inhibitors. These drugs enhanced serotonin activity and seemed to carry fewer side effects than other antidepressants. A famous development in the history of antidepressants, fluoxetine was approved by the FDA in 1987 and reached the market the following year as Prozac ® . A year later, almost 2.5 million prescriptions had been dispensed. Other SSRIs since released include paroxetine, sertraline, citalopram, escitalopram, and fluvoxamine.
https://www.greenbrooktms.com/blog/the-history-of-antidepressants
THE HISTORY OF DEPPRESSION
The earliest written accounts of what is now known as depression appeared in the second millennium B.C.E. in Mesopotamia. In these writings, depression was discussed as a spiritual rather than a physical condition. Like other mental illnesses, it was believed to be caused by demonic possession. As such, it was dealt with by priests rather than physicians.1
The idea of depression being caused by demons and evil spirits has existed in many cultures, including those of the ancient Greeks, Romans, Babylonians, Chinese, and Egyptians. Because of this belief, it was often treated with methods such as beatings, physical restraint, and starvation in an attempt to drive the demons out.
While many believed that demons were the root cause of depression, there were a number of ancient Greek and Roman doctors who believed that depression was a biological and psychological illness.
Greek and Roman doctors used therapeutic methods such as gymnastics, massage, diet, music, baths, and a medication containing poppy extract and donkey's milk to treat their patients.2
Hippocrates, a Greek physician, suggested that depression (initially called "melancholia") was caused by four imbalanced body fluids called humours: yellow bile, black bile, phlegm, and blood.2 Specifically, he thought that melancholia was caused by too much black bile in the spleen. Hippocrates' treatments of choice included bloodletting, baths, exercise, and diet.
A Roman philosopher and statesman named Cicero, in contrast, believed that melancholia had psychological causes such as rage, fear, and grief.
In the last years before the common era, in spite of some steps toward believing in more physical and mental causes of depression, it was still a very common belief among even educated Romans that depression and other mental illnesses were caused by demons and by the anger of the gods.
The Age of Enlightenment
During the 18th and 19th centuries, also called the Age of Enlightenment, depression came to be viewed as a weakness in temperament that was inherited and could not be changed. The result of these beliefs was that people with this condition should be shunned or locked up.
During the latter part of the Age of Enlightenment, doctors began to suggest the idea that aggression was at the root of the condition.5
Treatments such as exercise, diet, music, and drugs were now advocated and doctors suggested that it was important to talk about your problems with your friends or a doctor.
Other doctors of the time spoke of depression as resulting from internal conflicts between what you want and what you know is right. And yet others sought to identify the physical causes of this condition.
Treatments during this period included water immersion (staying underwater for long as possible without drowning) and using a spinning stool to put the brain contents back into their correct positions. Additional treatments included:
Diet changes
Enemas
Horseback riding
Vomiting
https://www.verywellmind.com/who-discovered-depression-1066770
MELANCHOLY (THE TERM FOR DEPRESSION IN THE PAST)
HISTORY OF DEPRESSION CONTINUES (follow red line)
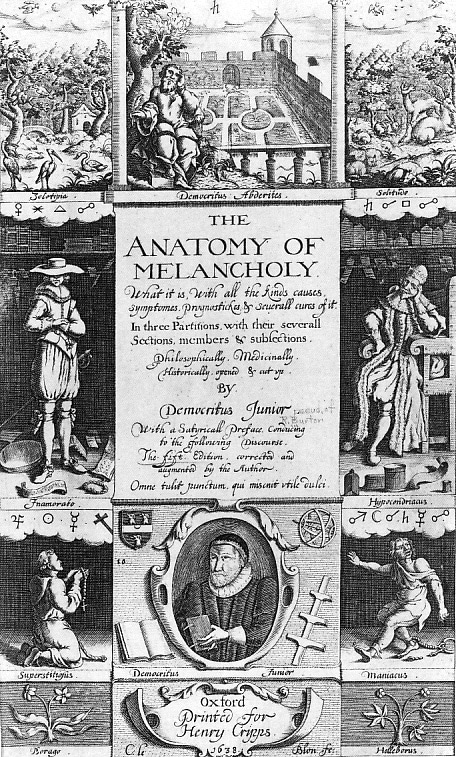

A Melancholic State of Mind
Considered the “Father of Medicine,” Hippocrates (460 – 370 BCE) was an ancient Greek physician who saw all bodily mechanisms as caused by the relative amount of four internal fluids, called humors: blood, black bile, yellow bile, and phlegm. He believed that a balance between the four brought on good health, while an extreme deficiency or excess of one caused physical ailments.
Greek physician and philosopher Galen (129AD – c. 200/c. 216) expanded upon Hippocrates’ theory, by stating that personality types were also derived from an excess of one of the four humors.
According to the humors theory, melancholic personality type was created by an excess of black bile. Melancholics were accordingly seen as introverted, deep thinkers, who typically related more to the sadder part of the emotional spectrum. It is from this perception of melancholia that our current concept of depression eventually evolved.
It was 19th Century German psychiatrist Emil Kraepelin who began referring to various forms of melancholia as “depressive states,” due to the low mood that defines it. Kraepelin also took a dual approach to mental illness, separating depression into two categories: manic depression and dementia praecox.
Sigmund Freud, the father of psychoanalysis, published his own thoughts on depression in his 1917 essay, Mourning and Melancholia. In it, Freud described melancholy in a similar manner to our current view on depression, elaborating that melancholy is defined by a sense of loss that arises when the object that has been lost is unknown, due to the mental process of repression.
Freud posited that depression interferes with the normal mourning process, causing the individual to feel a general sadness when coming in contact with the world at large, while experiencing the anguish and hopelessness assailing them as inescapable. Rather than internalize the positive aspects of the person or object that has been lost, and come to terms with their shortcomings, the person experiencing melancholy redirects any lingering resentment toward themselves, while maintaining the memory of their lost loved one as an ideal, untouchable version of who they were in real life.
Antidepressants affect the brain’s secretion of neurotransmitters, which are chemicals that relay information between nerve cells. Over the years, several generations of antidepressants have been approved and made publicly available, with each influencing the neural pathways involved in depression in a different way.
The three classes of antidepressants most commonly prescribed today are:
Tricyclic antidepressants (TCAs), which work on norepinephrine and were introduced in the late 1950s and early ‘60s. Examples include Elavil and Tofranil
Selective serotonin reuptake inhibitors (SSRIs), which were introduced in the mid-1980s. Examples include Prozac and Zoloft.
Serotonin and norepinephrine reuptake inhibitors (SNRIs), which were introduced during the mid-‘90s. Examples include Cymbalta and Effexor.
A
agomelatine
Allegron (see nortriptyline)
Alventa XL (see venlafaxine)
Amphero XL (see venlafaxine)
amitriptyline
B
Brintellix (see vortioxetine)
C
Cipralex (see escitalopram)
Cipramil (see citalopram)
citalopram
clomipramine
Cymbalta (see duloxetine)
D
Depefex XL (see venlafaxine)
dosulepin
doxepin
duloxetine
E
Edronax (see reboxetine)
Efexor XL (see venlafaxine)
escitalopram
F
Faverin (see fluvoxamine)
fluoxetine
fluvoxamine
Foraven XL (see venlafaxine)
I
imipramine
isocarboxazid
L
lofepramine
Lomont (see lofepramine)
Lustral (see sertraline)
M
Majoven XL (see venlafaxine)
Manerix (see moclobemide)
mianserin
mirtazapine
moclobemide
Molipaxin (see trazodone)
N
Nardil (see phenelzine)
nortriptyline
O
Olena (see fluoxetine)
Oxactin (see fluoxetine)
P
Parnate (see tranylcypromine)
paroxetine
phenelzine
Politid XL (see venlafaxine)
Prothiaden (see dosulepin)
Prozac (see fluoxetine)
Prozep (see fluoxetine)
R
reboxetine
S
Seroxat (see paroxetine)
sertraline
Sinepin (see doxepin)
Sunveniz XL (see venlafaxine)
Surmontil (see trimipramine)
T
Tonpular XL (see venlafaxine)
tranylcypromine
trazodone
trimipramine
V
Valdoxan (see agomelatine)
Venadex XL (see venlafaxine)
Venaxx XL (see venlafaxine)
Vencarm XL (see venlafaxine)
Venlablue XL (see venlafaxine)
venlafaxine
Venladex XL (see venlafaxine)
Venlasoz XL (see venlafaxine)
Venlalic XL (see venlafaxine)
Vensir XL (see venlafaxine)
ViePax XL (see venlafaxine)
vortioxetine
Z
Zispin (see mirtazapine)
ARE THERE DIFFERENCES AMONG ANTIDEPRESSANTS?
Antidepressants differ in their effects on neurotransmitters, established uses, adverse effects and drug interactions. All antidepressants that are used for depression are effective; there is no evidence that one antidepressant is more effective than another. However, patients may respond to or tolerate one antidepressant, and not respond to or tolerate another antidepressant.
WHAT ARE SIDE EFFECTS OF ANTIDEPRESSANTS?
Antidepressants that belong to the same class of antidepressant produce similar side effects. Antidepressants may cause withdrawal symptoms if abruptly discontinued. Withdrawal symptoms include nausea, vomiting, dizziness, headache, irritability, sleep disturbance, nightmares, psychosis, and seizures. All antidepressants have a warning about use in children and adolescents. Antidepressants increased the risk of suicidal thinking, and suicidal behavior in short-term studies in children and adolescents with depression and other psychiatric disorders. Anyone considering the use of antidepressant in a child or adolescent must balance this risk of suicide with the clinical need for the drug. Patients who are started on therapy should be closely observed for clinical worsening, suicidal thoughts or unusual changes in behavior.
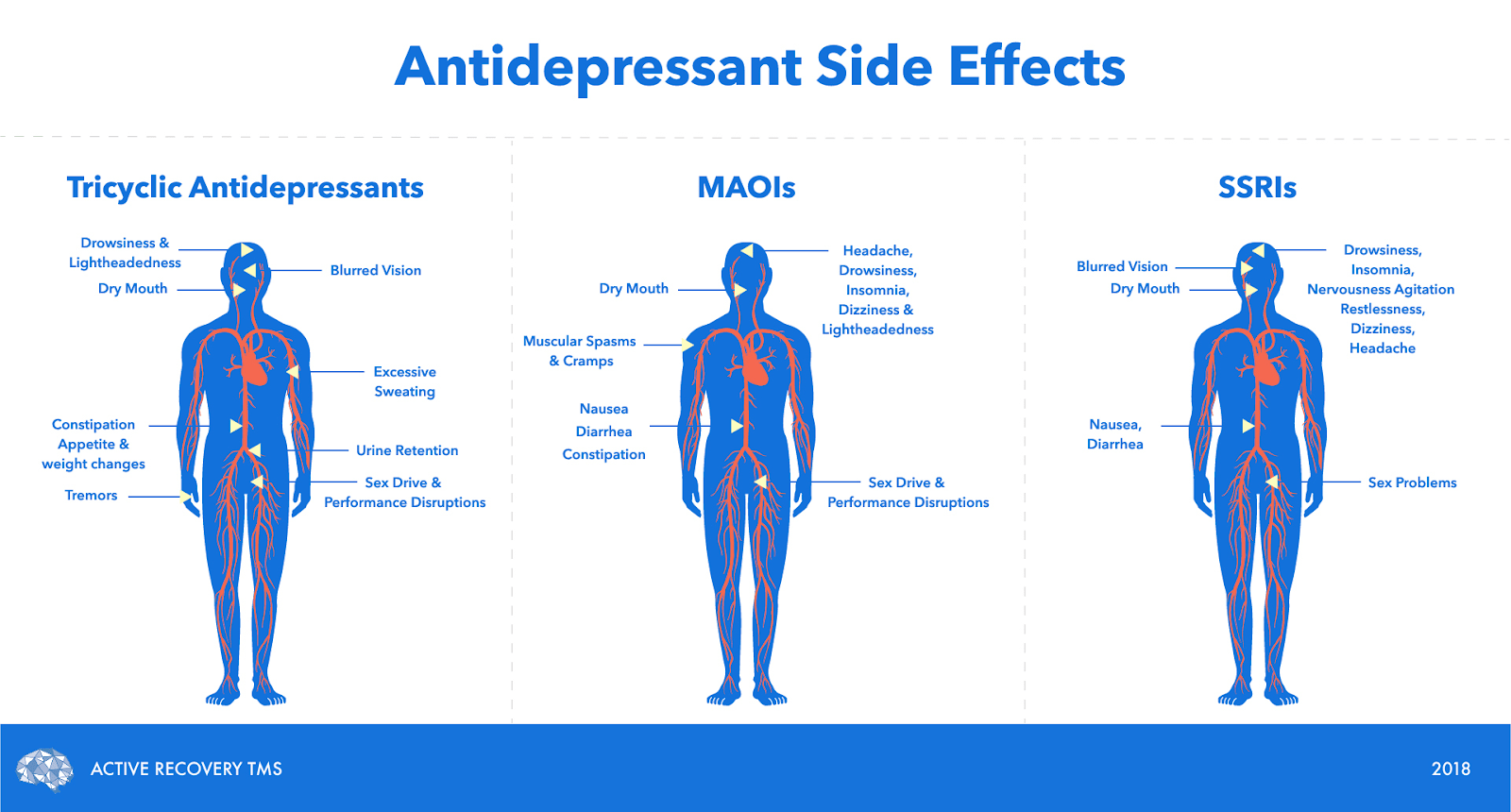
TRICYCLIC ANTIDEPRESSANTS (TCAS) SIDE EFFECTS
Tricyclic antidepressants (TCAs) are a class of antidepressant associated with sedation, dry mouth, blurred vision, constipation, urinary retention, and increased pressure in the eye. They are also associated with hypertension, abnormal heart rhythms, anxiety, insomnia, seizures, headache, rash, nausea, and vomiting, abdominal cramps, weight loss, and sexual dysfunction. Tricyclic antidepressants rarely cause liver failure.
SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIS) SIDE EFFECTS
Selective serotonin reuptake inhibitors (SSRIs) and serotonin/norepinephrine reuptake inhibitors (SNRIs) are two classes of antidepressants associated with abnormal thinking, agitation, anxiety, dizziness, headache, insomnia, sexual dysfunction, sedation, tremor, sweating, weight loss, diarrhea, constipation, dry mouth, rash, and nausea. Rarely, SSRIs have been associated with hyponatremia (low sodium), hypoglycemia (low blood glucose), and seizures.
MONOAMINE OXIDASE INHIBITORS (MAOIS) SIDE EFFECTS
Monoamine oxidase inhibitors (MAOIs) are a class of antidepressant associated with postural hypotension (feeling faint upon standing due to decreased blood flow to the brain), high blood pressure, fainting, abnormal heart rhythm, dizziness, headache, drowsiness, insomnia, anxiety, constipation, nausea, diarrhea, sexual dysfunction, weight gain or weight loss, and edema. Seizures, rash, blurred vision, and hepatitis are infrequently associated with MAOIs.
https://www.rxlist.com/antidepressants/drug-class.htm
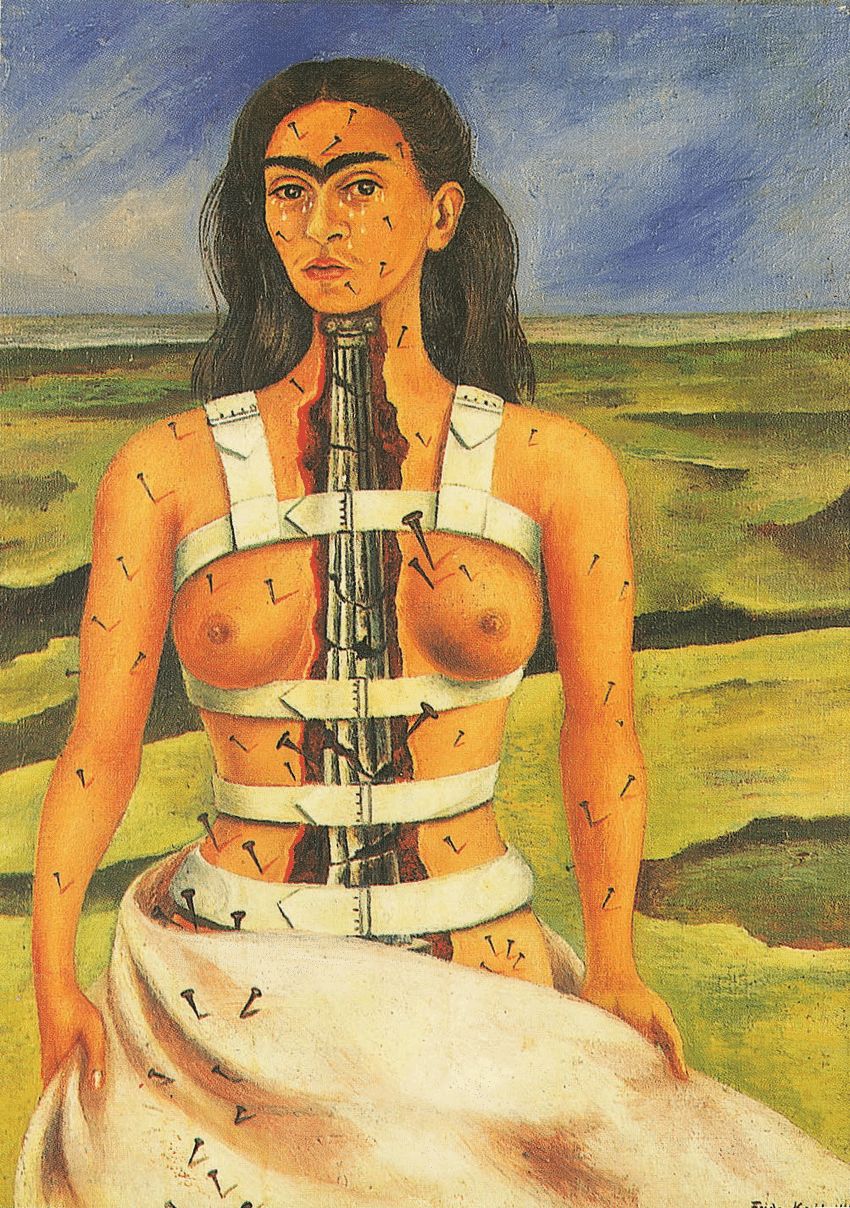
“I paint self-portraits because I am so often alone, because I am the person I know best.” -Frida Kahlo
Physical and mental suffering are strongly interconnected in her paintings; the accident had forever compromised Kahlo’s health and she had to have surgeries her whole life. “ The Broken Column” (1944) for example, shows us that she felt broken inside and outside as if the only thing that kept her together was the corset. Many spikes puncture her body, and her face is full of tears.
Kahlo was diagnosed with minor depression, but experienced two major depressive episodes and suicide attempts during her lifetime… Her apparent dissociation and identity issues lead many researchers and historians to believe that Kahlo suffered from an array of mental illnesses – from post-traumatic stress disorder to bipolar disorder to dissociative identity disorder.
I’m sad to have experienced the negative effects of medication, both around me as myself as well. As someone with multiple diagnosis of mental disorders, I have had quite a bit of therapy, but also have had medication myself. Where having a psychologist was extremely helpful, and helped me to live with myself, medication has had a negative effect. I had something called Stratera, and was used to help me with ADHD. It was taken once per day, in the morning. When I was on it, I didn’t notice all that much difference in my concentration. What I did notice, was having a slower reaction time, feeling muted and numbed. I lacked empathy, something that was a big personal trait of mine before I took medication. I had been on medication from 6 years old, till I decided to stop when I was 14. I took a pill, that changed from a person to more of a robot, every single day for 8 years. During those 8 years, my dose got increased 5 times. When I stopped, I started to experience being a person again. Sadly enough, I had also experienced a lot of trauma as a kid, and the medication muted a lot of the emotions back then. If I were to have the proper emotions at the time, and dealt with it in a healthy way, I think I would’ve been a healthier person today.
The next story is from an old close friend. He had severe social anxiety and depression. He would take medication to help supress the anxiety, just to be able to take the metro. Although it helped him at first, his anxiety got worse. So, he took more and more. Until he eventually spend the entire summer inside, taking 8 pills of Xanax per day. Before he was treated, he was an international DJ. Right now, I haven’t seen him in 3 years, and he hasn’t gone outside for anything besides walking the dog, which can still be too much. He is 30 years old.
But, there are also positive stories. I have also people around me with chronic depression. And were it not for their medication, they would’ve ended their life probably. People that are now at the happiest they’ve ever been, and more important, the most stable as well. Some have tried going of medication, because they didn’t want to be depended on pills. But this resulted in having relapses.
Medication can be extremely helpful, and sometimes even the only solution.
I think we do need to be more careful with who we give medication to, and why. And when we do, we need to monitor the dose and effectiveness accurately.
Personal experiences